Cooling for all and COVID-19
The pandemic, and the global response to it, will have profound implications for how we deliver critical services that rely on the ability to achieve cooling for all. The need to develop a vaccine is well understood, but the scope, requirements, and scale of cold chain and cooling solutions likely to be necessary to support a vaccine are not.
The COVID-19 pandemic that has dominated headlines since early 2020 has reshaped economic systems, changed human behaviour across the globe and demanded that the world rethink its response to climate change. Less widely appreciated are the impacts the pandemic has had on the developing world, how COVID-19 amplified other risks, and the opportunity to recover better with sustainable energy for all. The impact on poverty, for example, is stark. Due to COVID-19 alone, it is expected that at least 26 million people in Sub-Saharan Africa and 32 million people in South Asia will be forced into extreme poverty, measured at an income of USD 1.90 per day. [1]
Food systems and supply chains are being stretched and the ability of people to maintain nutritious diets will be negatively impacted by the economic downturn. When temperatures rise, social distancing will become much more complicated for those without access to cooling.
The drivers of change for cooling for all
Cold chain to deliver a vaccine
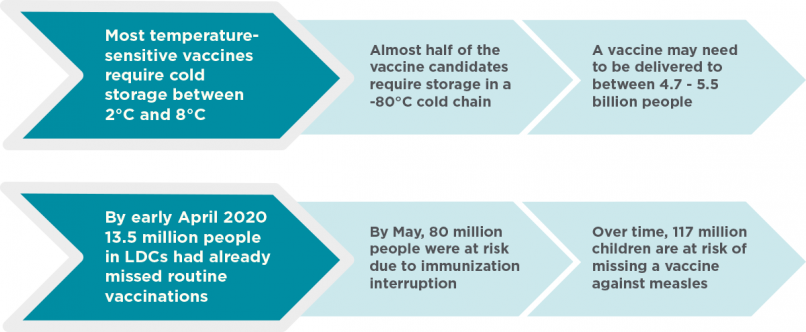
The global race to develop a vaccine for COVID-19 has preoccupied governments and the health community since the scale of the pandemic was realized. Considerably less attention has been paid to the cold chains that are likely to be necessary to deliver that vaccine. Close to half of the vaccine candidates currently in phase 1 or later trials will require storage in a -80°C cold chain, which would require building a new cold chain for low-income countries. [2] The temperature stability requirements of the vaccine candidates that receive approval are as yet unknown, but it is likely that at least the first approved vaccine will require some form of refrigeration.
Most temperature-sensitive vaccines, such as influenza vaccines, require cold storage between 2°C and 8°C. [3] Even if we are to build on the existing cold chain already in place for routine immunization, there are a number of issues that are key to understanding the scope of this challenge and the issues faced in the unprecedented attempt to reach an entire population, including the elderly or otherwise vulnerable, especially in low-income countries.
Twin challenges of delivering a COVID-19 vaccine
Prior to the pandemic, there were vast inequities in the health cold chain and challenges in achieving universal immunization coverage. In 2018, coverage for the vaccine protecting against diphtheria, tetanus, and pertussis (DTP3), which requires storage between 2°C and 8°C, was at 86 percent globally, meaning 19.4 million children went unvaccinated against preventable diseases. In Africa, coverage was only 76 percent, a figure that has plateaued since 2015. [4] Of the 10 countries that account for 60 percent of unvaccinated children, five are in the critical nine for access to cooling. [5]
60% of unvaccinated children live in 10 countries
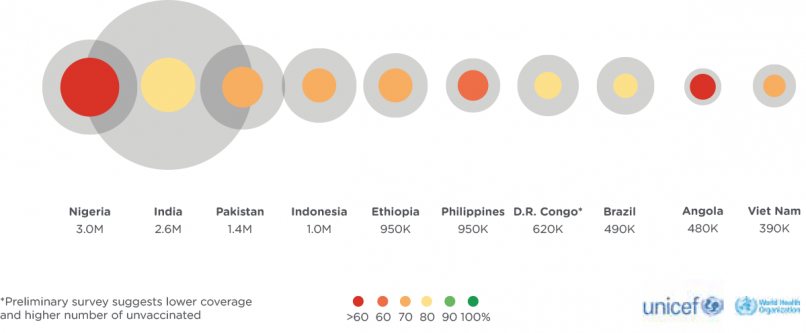
These inequities in delivering safe vaccines have been compounded by the COVID-19 pandemic. As of 3 April 2020, 13.5 million people in the world’s least developed countries (LDCs) had already missed routine vaccinations, risking their health and safety. [6] By mid-May 2020, it was estimated that 80 million children in 68 countries were at risk of diphtheria, measles and polio because of complications from the pandemic. Over time, 117 million children are at risk of missing another temperature-sensitive vaccine against measles [7], compared to 182 million children who missed the vaccine between 2010 and 2018. [8]
These challenges are immense and will be compounded further if the delivery of a COVID-19 vaccine to 60–70 percent of the population, or 4.7–5.5 billion people, is dependent on cold chain capacity. [9] To put the development challenge into perspective, since its launch in 2000, Gavi has helped vaccinate more than 760 million children. A 2017 study on cold chain availability showed that only 10 percent of health facilities in Gavi-supported countries were equipped with the recommended cold chain equipment. [10] The remainder lacked functional devices or were equipped with poor performing devices. Not only will massive amounts of new cold chain equipment be necessary, but difficult trade-offs between the delivery of the vaccine and other temperature-sensitive vaccines and medical products could also be required.
Further complicating the delivery of a COVID-19 vaccine is the lack of reliable electricity supply in rural hospitals and health clinics. In Ghana, for example, only 27 percent of health facilities have stable access to electricity and in Uganda the figure is 29 percent. [11] Across Sub-Saharan Africa only 28 percent of healthcare facilities enjoy the reliable electricity supply that is necessary to keep vaccines cool and power ventilators. [12]
Other gaps in the current routine immunization system will most certainly be exacerbated. These include transport and delivery capacity at the last mile to ensure potency, where the volume and effectiveness of cold packs play a crucial role. In addition, most low-income countries rely on campaign and outreach models for distributing vaccines, especially during outbreaks. This will most likely also be the case for COVID-19 vaccines. Such efforts require some form of cooling, often off-grid and powered by ice, in order for health care workers to travel to communities in order to deliver much needed vaccines.
Nutritional preferences and malnourishment
Access to cooling, in terms of commercial and household cold storage and cold chains, is necessary to support changing consumer preferences and behaviour during and after the pandemic. Refrigeration of food prevents spoilage, reduces trips to the market, and supports a healthy diet. A recent survey of Asian countries found an increase in the consumption of food products that are perceived to be healthy, notably fresh foods that require cold chains to maintain their nutritional value. [13]
Consumer spending elsewhere is expected to follow suit. In India, for example, 34 percent of households reported that they now anticipate spending 20 percent of their income or more on fresh food than they did prior to the pandemic, with that number increasing to 52 percent after the pandemic vs. during. Yet the necessary infrastructure is lacking to support increased demand. India loses approximately 18 percent of its domestic production of milk, meat, seafood, fruit and vegetables due to a lack of cold chain [14], and only 30 percent of Indian households have access to a refrigerator. [15]
Nutritional preferences and food loss due to lack of cold chain
|
Country |
% of respondents selecting stable availability of fresh food products among top 3 factors for store selection |
Anticipated consumption of fresh foods during COVID-19 (% of households reporting an increase in spending of 20% or more) |
Anticipated consumption of fresh foods after COVID-19 (% of households reporting an increase in spending of 20% or more) |
Production of milk, meat, seafood, fruit and vegetables lost due to lack of cold chain |
|---|---|---|---|---|
|
India |
39% |
34% |
52% |
18% |
|
Indonesia |
41% |
31% |
30% |
22% |
|
Thailand |
34% |
23% |
14% |
22% |
These trends, however, account only for consumer preferences and the baseline of existing cold chain systems, and not for the expected impact of increased poverty. Previous research has shown that in poor countries, calories from nutritious foods are often as much as 10-times more expensive than cereals or grains in caloric terms, and when faced with significant reductions in income vulnerable groups typically prioritize less nutritious foods with higher caloric value. [16] As a result of the crisis, an estimated 320 million children have lost their access to school meal programmes, with rural households feeling the effects more acutely. [17] Prior to the pandemic, 135 million people, including 73 million in Africa, were facing crisis or emergency levels of food insecurity. [18] Should the pandemic produce a reduction on global GDP between 2 percent and 10 percent, the number of undernourished people in net-food importing countries could increase from 14.4 to 80.3 million. [19]
The economic impact on smallholder farmers reliant on the production and sale of goods requiring cold storage for their incomes and livelihoods is another key issue exacerbated by COVID-19. Among other issues, access to trade routes and labour has been reduced as a result of social distancing measures. In Ethiopia, prices for vegetables are declining and there are examples of farmers leaving fresh crops to rot due to a lack of markets. [20]
Finding social distance when temperatures rise
On 28 April 2020, at the height of the pandemic, Delhi recorded its highest temperature of the year at 43.7°C, eclipsing the previous hottest day of 42.1°C five days earlier on April 23. [21] Later in May, nearly 80 migrant workers in India died of starvation or heat stress while moving from crowded cities to their home villages. [22] The health and economic risks of heat stress are well known – declining productivity, safety concerns for vulnerable groups, and higher peak energy demand – but will be exacerbated by a pandemic response that requires social distancing, particularly for those who already lack access to cooling. The amplified risks of hot weather are summarized concisely by the Global Heat Health Information Network:
-
Many vulnerable groups are susceptible to both heat stress and COVID-19, including the elderly, those with pre-existing health conditions, limited access to healthcare, or those living in poor quality housing
-
People at risk in hot weather may see an already precarious socioeconomic condition exacerbated by COVID-19
-
Inhabitants of dense urban centres with limited green space have amongst the worst COVID-19 outcomes due to pre-existing exposure to air pollution and high rates of non-communicable diseases
-
Inhabitants of slums and informal urban settlements will not be able to stay indoors during a heatwave due to an inability to cool their homes. [23]
Consider a crowded urban slum experiencing a heatwave. Housing quality is likely to be low, with higher temperatures brought on by corrugated metal roofs and the urban heat island effect, and intermittent electricity access that means families cannot rely on electrical cooling devices, such as fans. In these circumstances, common responses cannot be reconciled with public health measures needed to prevent COVID-19 transmission, including public cooling centres, gathering in green spaces, checking on vulnerable people, and seeking medical care if necessary.
Recover better with cooling for all
Guarantee a vaccine with sustainable cold chain
Delivering a vaccine that must be kept between 2°C and 8°C to 4.7–5.5 billion within 12–18 months will require a massive expansion in health cold chain infrastructure. As with efforts to develop vaccine manufacturing capacity prior to its discovery, cold chain infrastructure investment must begin immediately – to serve both ongoing and pandemic-related cooling needs. In order to prevent a lock-in of highly inefficient technologies that are procured on an expedited basis, countries, philanthropies and development institutions must utilize procurement standards that prioritize affordable, energy-efficient equipment powered by renewable energy that meets the standards of the Kigali Amendment to the Montreal Protocol.
Existing platforms must be leveraged and scaled up. Gavi’s Cold Chain Equipment Optimisation Platform (CCEOP) has already committed USD 250 million and delivered over 60,000 new pieces of cold chain equipment over the past two years. [24] At the same time, we must invest in data and monitoring tools to understand the scope of cold chain gaps, where and why they break down, as well as the human resources necessary to maintain the equipment into the future. Gavi launched INFUSE – Innovation for Uptake, Scale and Equity in Immunization – to focus on high-impact innovations for addressing country-level needs and in collaboration with Nexleaf Analytics that is developing the Intelligent Maintenance and Planning Tool (IMPT), which aims to integrate data across GAVI countries. As demand and price of vaccines increase, and with them the volume of equipment procurement, monitoring is necessary in order to make the deployment manageable, cost-effective and right-sized.
These cooling efforts must be aligned with energy access strategies, including stimulus efforts to recover better with sustainable energy for all. Hospitals and clinics must be guaranteed the energy necessary to power additional cooling needs with renewable energy. Demand-side solutions to maximize energy efficiency and cooling solutions that use no energy can help reduce these added energy requirements.
Using sustainable cold chain to recover better in agriculture
Data gaps in agricultural cold chains can be filled with rapid assessments and recovery packages can invest in the delivery of sustainable cooling technologies to ensure functioning supply chains for nutritious food. The FAO has called for assessments of food stocks and yields to determine gaps, surpluses and potential shortages, as well as taking inventory of cooling infrastructure and cold chains. [25] With these data in hand, investment in an increasing supply of sustainable cooling solutions for the agricultural cold chain can be leveraged through trade and public procurement policies, among others. In low-income countries, interventions are needed to provide cold storage directly after production and at the last mile. Training programmes for installation and maintenance of cooling equipment and resources in off-grid communities are fast ways to boost economic activity and create new jobs.
Governments and multilateral development institutions can also use the social programmes and finance at their disposal to improve the nutritional quality of diets and stimulate demand for nutrient-rich foods, both in terms of the immediate economic stimulus and recover better efforts. Levers include cash transfers, communications campaigns, and social protection programmes.
Protecting the vulnerable from heat stress and COVID-19 simultaneously
There are practical steps countries and cities can take. The WHO has recommended the implementation of heat-health action plans, including a specific review for 2020 that considers the implications of the pandemic and strategies to reduce and prevent COVID-19 transmission. [26] The Global Heat Health Information Network has prepared a planning checklist to guide this process [27], and key among the actions is providing practical information on how vulnerable groups can protect themselves from both heat stress and COVID-19 simultaneously.
Local and national governments also have an important role in educating the public on affordable and sustainable cooling solutions and providing the financial and technical support necessary to ensure vulnerable groups can access them. This includes efforts that make efficient fans more accessible, such as the Global LEAP results-based financing facility that resulted in more than 193,000 verified fan sales in developing markets. [28] It may also require financial tools to make efficient air conditioning or refrigeration more affordable, particularly in the light of economic recession, and proactively implementing evaporative cooling and passive cooling solutions in buildings, including cool roofs, shading and vegetation.