Cooling for health services

|
Chapter 2.2 Chapter 2 overview |
Key messages
- We cannot deliver SDG3 (good health and well-being) without sustainable cold chains that guarantee vaccines, and comfort cooling that ensures effective care in hospitals and health centres.
- Immunization is one of the most effective public health interventions for protecting lives globally and relies on access to both electricity and cooling.
- The COVID-19 pandemic has shown us exactly why we need to extend sustainable vaccine cold chains to rural health clinics.
20%
of health facilities did not have access to cold chain equipment in 57 Gavi-eligible countries.
260,000
African children are killed by malaria each year. The new, temperature-sensitive malaria vaccine will need functioning cold chains.
10%
of the power capacity of a conventional vaccine refrigerator is required by super-efficient refrigerators.
Overview
Access to sustainable cooling underpins the delivery of important components of SDG3 (good health and well-being) due primarily to the cooling needs of vaccines and blood products, as well as the need to regulate temperatures in hospitals and rural health clinics. The ability to cool hospitals, vaccines and other medical products is also typically enabled by access to electricity, highlighting the close link between SDG7 and sustainable cooling for all.
The cooling needs in health services include cold chains that transport temperature-sensitive medical products. Vaccines must typically have consistent cold storage between 2°C and 8°C to maintain their efficacy, with the exception of vaccines that require ultra-cold chain (UCC) storage of -20°C to -70°C, as was the case for the initial storage of some COVID-19 vaccines (e.g., those produced by Moderna and Pfizer-BioNTech). Blood, insulin and some medicines also require cooling, with blood, for example, stored between 2°C and 6°C, and fresh frozen plasma stored at below -30°C. Many sterilants and disinfectants must be stored below 30°C, with their effectiveness weakening when ambient temperatures are too hot. Additional cooling needs in the health sector include temperature control in hospitals and rural health centres that support better overall care and patient recovery through reductions in heat stress among patients and staff.
Vaccines
Vaccines are highly temperature sensitive. Prolonged exposure above 8°C, any exposure above 20°C, and accidental freezing can all damage or destroy vaccines. In some instances, ineffective vaccines can unknowingly be administered, leaving recipients exposed to deadly disease. Approximately 5 million children under the age of five die every year, [1] and it is estimated that 1.5 million deaths could be avoided annually through improved vaccine coverage. [2] As such, sustainable cold chains are a necessary tool in the effective delivery of immunization programmes.
Outside COVID-19 vaccination efforts, immunization coverage rates are not keeping pace with population growth and have likely been hampered by efforts to address the COVID-19 pandemic. In 2020, the World Health Organization (WHO) reported that global coverage for the three-dose diphtheria-tetanus-pertussis vaccine (DPT3), which protects against a variety of infectious diseases, fell from 86 percent to 83 percent. This leaves 17.1 million children without an initial dose of DPT3, with an additional 5.6 million children only partially vaccinated. Among the 54 high-impact countries for access to cooling, 12 reported that more than 30 percent of children missed the third dose of the DTP vaccine between 2019 and 2020.
Figure 2.11: Percentage of children who missed the third dose of DTP vaccine (2019–2020)
Data availability continues to be a challenge for effectively identifying vaccine cold chain gaps, however a 2014 survey among 57 Gavi-eligible countries provides a valuable baseline, finding that up to 90 percent of health facilities did not have access to reliable cold chain equipment that could guarantee vaccines were not exposed to excessive heat or excessive freezing, including 20 percent without any cold chain equipment at all (Figure 2.12). [3]
Figure 2.12: Survey of cold chain equipment in 57 Gavi-eligible countries
WHO's Effective Vaccine Management (EVM) assessment from 2009–2020 reveals that no service points or local distribution in any of the 86 countries surveyed had storage facilities capable of maintaining temperatures of -20°C. Further, only 1 percent of service points stored vaccines in cold/freezer rooms or received vaccines from refrigerated vehicles (Figure 2.13). [4] This points to challenges with access to cooling in last-mile locations in countries covered by the assessment.
Figure 2.13: Cold chain indicators for 86 countries
COVID-19
New equipment enables greater access to cooling in the short term and the cold chain infrastructure needed to support routine immunizations and other health care needs in the long term. WHO and the UN set a global COVID-19 vaccination target of 70 percent by mid-2022, noting that sufficient supply from the manufacturers was available to meet those targets, if equitable distribution was also possible. [5] With loosening supply constraints and cold chain progress, COVAX [6] now expects to reach a key milestone of over 2 billion doses [7] released for delivery. However, access inequities remain, with only 14.4 percent of people in low-income countries having received a first dose of a COVID-19 vaccine. [8]
The US Centers for Disease Control (CDC) has supported additional progress through better data by verifying that vaccines from Pfizer-BioNTech and Moderna can be stored at higher temperatures (of between 2°C and 8°C) for approximately 30 days rather than what was initially thought (-70°C and - 20°C respectively) (Table 2.1). In countries with limited capacity for UCC, particularly in rural areas, these data enable medium-distance distribution, improving vaccine accessibility.
Table 2.1: Maximum storage durations at select temperatures
|
Efforts to Scale Up Ultra-Cold Chain Capacity in Bangladesh On behalf of COVAX, UNICEF initiated a project in 2021 to deliver more than 350 UCC freezers, some of which can store up to 336,000 vaccines, to more than 45 countries. This included Bangladesh, where through COVAX, UNICEF shipped 26 large freezers, increasing its UCC capacity by the equivalent of almost 9 million vaccines. [9] By the end of March 2022, Bangladesh had provided the second vaccine dose to just over 107 million people, or around 63 percent of the total population, with a notable increase in vaccine uptake in March 2022. [10] Through bilateral and multilateral agreements, donations, and the COVAX facility, the country has received 467.6 million total doses of vaccines, including 138 million (approximately 30 percent) Moderna or Pfizer-BioNTech vaccines requiring UCC. [11] With approximately 47.3 million doses requiring UCC already administered, additional UCC capacity, and higher short-term temperature requirements for mRna vaccines, Bangladesh saw a significant increase in the administration of first, second and third doses of the Pfizer-BioNTech vaccine in early 2022. [12] |
Malaria
SDG3 includes a target for ending diseases such as malaria, AIDS and tuberculosis by 2030. Yet malaria is on the rise, increasing by 14 million cases and 47,000 deaths from 2019 to 2020. [13] In Sub-Saharan Africa malaria is the primary cause of death and childhood illness, killing 260,000 African children each year. [14]
Malaria was historically treated with antiviral medications that do not require cooling, but recent vaccine developments have made cold chains an essential component of the malaria response, with the RTS,S/AS01 (RTS,S) malaria vaccine (stored between 2°C and 8°C ) recommended for children in Sub-Saharan Africa. [15] [16] The vaccine was trialled with 2.3 million doses in three pilot countries, where it resulted in a 30 percent reduction in deadly malaria, and saved one life for every 200 children vaccinated. [17]
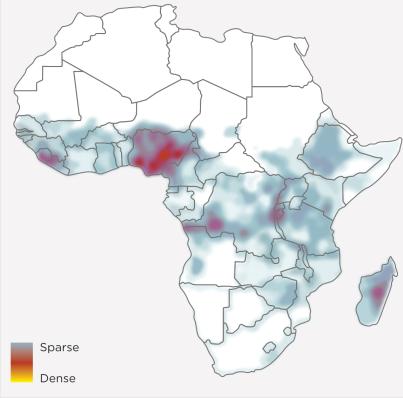
In 2020, 10 countries in Sub-Saharan Africa accounted for 68 percent of malaria cases and 71 percent of deaths from malaria (Figure 2.14). With the exceptions of the Democratic Republic of the Congo and Tanzania, they are all high-impact countries for access to cooling, including Nigeria and Mozambique that are also among the Critical 9 countries.
Figure 2.14: Top 10 countries for global malaria cases and deaths in 2020
Cooling in hospitals and health centres
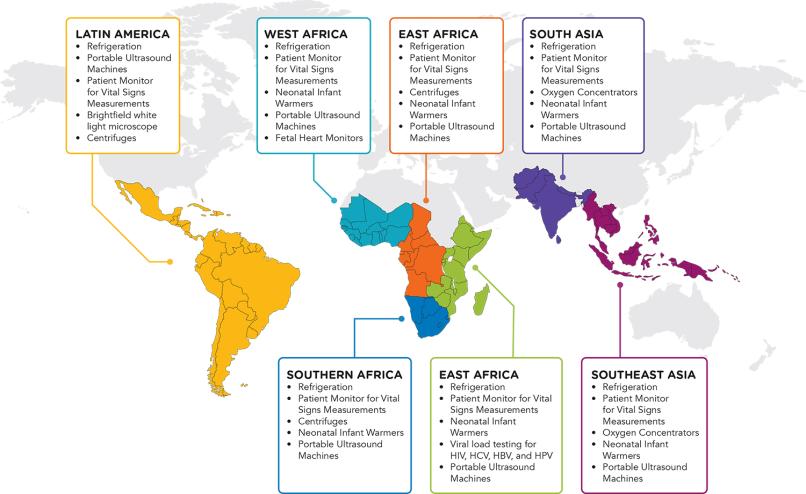
Well-functioning medical cold chains and access to refrigeration in health facilities are crucial to ensure the preservation of vaccines, blood products and medicines until they reach their target populations. In the 2018 Efficiency for Access Off-Grid Appliance Market Survey, refrigerators for vaccines and blood banks were the top items of medical equipment by perceived demand in all regions, [18] which suggests a persistent gap despite many initiatives seeking to provide off-grid clinics with refrigeration options.
Another important aspect of cooling in health centres is the presence of fans or air conditioners to reduce the adverse effects of heat on vulnerable people, especially in regions with warm and humid climates. Fans, for example, are proven effective to prevent heat-related stress and mortality in hospitals during severe heat waves, and to reduce exposure to disease-carrying insects and the spread of mould allergens. [19] Looking ahead, in a warming world, the availability of reliable space cooling and refrigeration will become increasingly vital to ensure the resilience of health services during heat extremes.
Figure 2.15: Ranking of relative demand for medical equipment by region [20]
While passive cooling can reduce energy demand for cooling in health care settings, access to electricity is a necessary precondition for hospitals and health facilities to meet their cooling needs. Electricity underpins most requirements of a well-functioning health centre, from using modern equipment for medical procedures, to communication, sanitation and hygiene, lighting and facility operations as well as refrigerators, fans and air conditioners. [21]
In Gujarat, India, the state government rural electrification programme Jyotigram Yojana (JGY) introduced 24-hour electricity access to rural non-agricultural users including schools, small commercial enterprises and health centres across the state with the goal of reducing service interruptions in these settings. The programme resulted in improved cooling capacity for health facilities, with the probability of having a functioning deep freezer, ice-lined refrigerator, cold box, and vaccine carrier increasing between 5.2 and 6.6 percent.
Reliability of power supply is fundamental, yet on average, 51–67 percent of health facilities experience voltage fluctuations of at least 15 percent. [22] Cooling equipment such as ceiling fans and refrigerators for vaccines are often able to withstand moderate voltage fluctuations following power outages. [23] However, intermittent power can limit services, create facility hazards, [24] and contribute to cooling equipment breakdown.
Figure 2.16: Voltage fluctuation indicators from the WHO EVM Assessment
Nearly 59 percent of over 121,000 health care facilities analyzed in 2018 in 46 low- and middle-income countries lack access to reliable electricity (Figure 2.16). [25] In areas with weak or no grid connection, decentralized and off-grid renewable energy can provide reliable electricity, and do so with rapidly deployable, cost-effective solutions. [26] In most cases, solar PV technologies can supply electricity at lower cost than diesel generators – a solution many off-grid health centres utilize. [27]
Even in medium-sized off-grid health care facilities, the most appropriate energy solutions are often hybrid, combining renewable technologies with efficient batteries and back-up generators, depending on the availability and cost-effectiveness of different power solutions. [28] A recent study estimated that solar PV and battery storage would be cost-effective for 50,000 off-grid health care facilities in Sub-Saharan Africa and improve proximity of health care services for 281 million people, reducing travel time to health care facilities by 50 minutes on average. [29]
Figure 2.17: Health care facilities with no detected electricity access [30]
Where power supply is constrained, energy-efficient cooling solutions allow health centres to make the most of available electricity capacity. At the same time, energy-efficient appliances can help them provide health services at lower costs.
Solutions for health services
Passive solutions, such as natural ventilation and shading, can help meet cooling needs and minimize energy demand in health centres. For example, the Friendship Hospital Shyamnagar, a small facility in the coastal district of Satkhira in south-western Bangladesh, was awarded as “best building in the world” in 2021 by the Royal Institute of British Architects thanks to its climate-conscious design: the hospital’s buildings take advantage of wind to encourage cross-ventilation and ensure shading from direct sun while also maximizing natural light. As a result, the need for air-conditioning is limited to operating theatres and delivery rooms. [31]
Nature-based solutions, such as trees and water, can reduce temperatures in health facilities, improving care and lowering energy needs. In Singapore, the Changi General Hospital installed a garden on the roof, and together with water features and energy-efficient cooling devices and techniques, saved the facility USD 800,000 in annual energy and water costs. Without consideration of these types of solutions, health centres can become heat sinks that require resources to pay for energy that can otherwise be directed to better care. [32]
Efficient cooling appliances, such as refrigerators or air conditioners, can meet any cooling needs not met by passive or nature-based solutions. In off-grid primary health centres, refrigerators can have relatively high electric loads, and appliance efficiency can make a substantial difference. Super-efficient refrigerators require only 10 percent of the power capacity of a conventional vaccine refrigerator, allowing the same energy system to supply energy to a larger set of appliances and medical devices at the same time. [33]
In the vaccine cold chain, advances in refrigeration have helped improve reliability for the storage of vaccines in weak- or off-grid settings. Solar direct drive (SDD) refrigerators have become a more reliable option than earlier solar battery refrigerators and are more sustainable than older fridges supported by kerosene or gas. [34] Bulk public procurement of high-standard equipment by governments for the most sustainable refrigeration technologies is a key mechanism to finance these solutions in developing markets.
Figure 2.18: Energy system needed to support a conventional or super-efficient solar refrigerator

Notes and references
[1] UNICEF. Levels and trends in Child Mortality, December 2021. Link.
[2] WHO. Immunization Agenda 2030: a global strategy to leave no one behind. Geneva: WHO; 2020. Link.
[3] Cold Chain Equipment Optimisation Platform, Gavi the Vaccine Alliance, December 2020. Link. Pg. 2.
[4] EVM Global Data Analysis, WHO, 2020. Link. Pg. 27.
[5] Strategy to Achieve Global COVID-19 Vaccination by mid-2022, WHO, 7 October 2021. Link. Pg. 7.
[6] COVAX is a global initiative that is working with governments and manufacturers to ensure COVID-19 vaccines are available worldwide to both higher-income and lower-income countries. It is co-convened by the Coalition for Epidemic Preparedness Innovations (CEPI), Gavi, the Vaccine Alliance and WHO – working in partnership with UNICEF as a key implementing partner, developed and developing country vaccine manufacturers, the World Bank and others.
[7] UNICEF COVID-19 Vaccine Market Dashboard (data collected March 2022). Link.
[8] Hannah Ritchie, Edouard Mathieu, Lucas Rodés-Guirao, Cameron Appel, Charlie Giattino, Esteban Ortiz-Ospina, Joe Hasell, Bobbie Macdonald, Diana Beltekian and Max Roser (2020) – "Coronavirus Pandemic (COVID-19).” Link.
[9] The historic push to provide ultra-cold chain freezers around the world, UNICEF, 20 September 2021. Link.
[10] COVID-19 Vaccination Dashboard for Bangladesh, Government of Bangladesh.
[11] UNICEF COVID-19 Vaccine Market Dashboard (data collected March 2022). Link.
[12] COVID-19 Vaccination Dashboard for Bangladesh, Government of Bangladesh. Link.
[13] World Malaria Report 2021. WHO, 6 December 2021. Link. Pg. vi.
[14] WHO Recommends Ground-breaking Malaria Vaccine for Children at Risk. WHO, 6 October 2021. Link.
[15] WHO Recommends Ground-breaking Malaria Vaccine for Children at Risk. WHO, 6 October 2021. Link.
[16] Fortpied, J., Collignon, S., Moniotte, N. et al. The thermostability of the RTS,S/AS01 malaria vaccine can be increased by co-lyophilizing RTS,S and AS01. Malar J 19, 202 (2020). Link.
[17] World Malaria Report 2021.WHO, 6 December 2021. Link. Pg. 9.
[18] Off-Grid Appliance Market Survey 2018. Efficiency for Access Coalition. Link.
[19] Fans: Solar Appliance Technology Brief, Efficiency for Access Coalition, May 2021. Link.
[20] Off-Grid Appliance Market Survey 2018. Efficiency for Access Coalition. Link.
[21] Impact Factsheet: Health Facility Electrification and Health Outcomes. SEforALL, 2022. Link.
[22] Effective Vaccine Management Assessment 2009–2020. WHO. Link.
[23] Franco A., Shaker M., Kalubi D., Hostettler S., A review of sustainable energy access and technologies for health care facilities in the Global South, Sustainable Energy Technologies and Assessments, Vol. 22, 2017.
[24] Cronk R, Bartram J. Environmental conditions in health care facilities in low- and middle-income countries: Coverage and inequalities, International Journal of Hygiene and Environmental Health, Vol.221, Issue 3, 2018.
[25] Cronk R, Bartram J. Environmental conditions in health care facilities in low- and middle-income countries: Coverage and inequalities, [1] International Journal of Hygiene and Environmental Health, Vol. 221, Issue 3, 2018.
[26] Off-Grid Renewables Supply: Life-Saving Power to Rural Health Centres. IRENA, 2018. Link.
[27] Porcaro, Jem et al. “Lasting Impact: Sustainable Off-grid solar delivery models to power health and education,” UN Foundation and SEforALL, 2019. Link.
[28] Franco A., Shaker M., Kalubi D., Hostettler S., A review of sustainable energy access and technologies for health care facilities in the Global South, Sustainable Energy Technologies and Assessments, Vol. 22, 2017.
[29] Moner-Girona M., Kakoulaki G., et al. Achieving universal electrification of rural health care facilities in Sub-Saharan Africa with decentralized renewable energy technologies. Joule. Vol. 5, Issue 10, 2021.
[30] Moner-Girona M., Kakoulaki G., et al. Achieving universal electrification of rural health care facilities in Sub-Saharan Africa with decentralized renewable energy technologies. Joule. Vol. 5, Issue 10, 2021.
[31] Friendship Hospital Wins Riba Prize 2021. Friendship NGO. 2021. Link.
[32] Healthy Hospitals, Healthy Planet, Healthy People: Addressing Climate Change in Health Care Settings, WHO Discussion Draft. Link.
[33] Energy Efficiency and Health Access: A Preliminary Assessment, Efficiency for Access Coalition, 2018. Link.
[34] Port to patient: Improving country cold chains for COVID-19 vaccines, McKinsey. Link.