Sustainable cold chains needed for equitable COVID-19 vaccine distribution
By Toby Peters, Professor, University of Birmingham and Ben Hartley, Energy Efficiency Specialist, SEforALL
This article is a summary of the Cooling for All: The role of cold chain in delivering a COVID-19 vaccine briefing note, produced by Sustainable Energy for All (SEforALL), University of Birmingham, Nexleaf Analytics, the International Institute for Energy Conservation, and the Basel Agency for Sustainable Energy. Read the full briefing note here.
The COVID-19 pandemic has changed life on a massive scale, disrupting economies, communities and families. Lockdowns, social distancing and isolation have been the first tools deployed by governments around the world in their fight against the pandemic and a vaccine is seen as the decisive next move to get societies back on their feet and economies running. The distribution of the vaccine to every remote village, especially in low- and middle-income countries, has been recognized as a key issue of equity that would prevent 61 percent of subsequent deaths, compared to 33 percent of deaths avoided if the vaccine is distributed to high-income countries first.
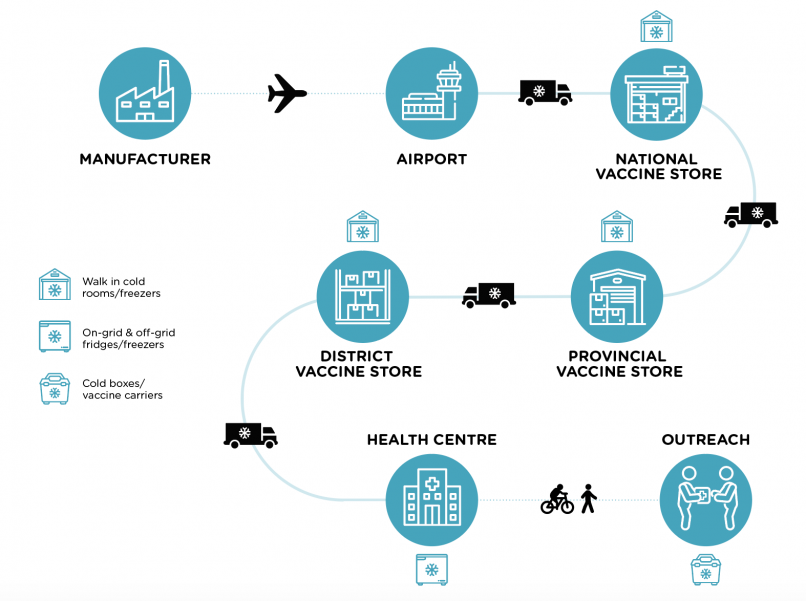
Once a vaccine is approved, equitable distribution is highly likely to be reliant on a dramatic expansion of cold chains across the developing world. Most leading vaccine candidates require cooling between 2°C and 8°C, and the first COVID-19 vaccine to announce efficacy results from mass testing requires cold storage at -70°C. Put simply, access to sustainable medical cold chains will likely underpin equitable global distribution. As the world manages the necessary and urgent expansion of these cold chains, we must ensure the investment relies on sustainable solutions and delivers a lasting legacy.
Cold chain is the missing piece of the planning
Efforts to find a lasting solution to the COVID-19 pandemic are primarily focused on developing, testing and manufacturing an effective vaccine. Little attention to date has been given to the requirements for distributing it rapidly at scale. It is estimated that 60–70 percent of the population will need a vaccine to develop herd immunity. If a vaccine requires two doses, over 10 billion vaccinations could be needed. Such unprecedented volume and velocity of mass vaccination will require a new fast-track approach. To complicate matters further, many of the leading vaccine candidates require cold storage between 2°C and 8°C, and the first vaccine candidate announced to be effective, from Pfizer-BioNTech, requires two doses and cold storage at -70°C. Central to any vaccine distribution plan will be the cooling equipment and cold-chain infrastructure which in the developing world will require re-engineering and significant new capacity.